Yes they do all go together in one sentence. I never thought this would be a subject I would really openly talk about but thanks to a chat with the amazing @msgracefullnot via video call, I feel more able to open up and talk about my experiences.
Having a neurological condition (or 2) has knock on effects that vary from person to person so please don’t think that what has happened to me will necessarily happen to you.
As you are probably all aware by now I have Transverse Myelitis and Relapse-Remitting Multiple Sclerosis. Both have similar characteristics although I have 3 areas that led to the diagnosis of these conditions.
Transverse Myelitis was diagnosed in Jn 2016 after having an MIR scan that showed a complete lesion across T1 on my spinal cord and an incomplete lesion at C3. The lesion at T1 has caused me to lose all sense and feeling from my bra line down meaning I cannot feel my legs or feet and I have no awareness of my bladder or bowel.
The incomplete lesion at C3 has caused alters sensations in my arms, specifically my right side,leading to pins and needles and numbness.
9 months after my TM diagnosis I was diagnosed with RRMS. This was confirmed after numerous blood tests, lumbar puncture and another MRI with contrast. Tbis highlighted that I had 3 subcortical white matter lesions that were active along with a number of non-active/scar like lesions across the white matter of my brain.
The combination of all these lesions has lead to me having lost the ability to walk and also long standing problems with my bladder and bowel.
As a parent I’m used to talking to other mums about poo and the like so sharing my personal experiences will either be a breeze or a major disaster so please bear with me.
When I first lost all my feeling it happened over a few hours starting from my thighs down and worked it’s way up to my bra line. It was an incredibly scary time. No-one knew what was happening and it drove me crazy. Whilst I was in A&E it dawned on me that I hadn’t actually passed urine in 4 hours and I was resembling a beach ball as my bladder filled and for some unknown reason (I know now) I had gone into urinary retention. I had a 14fr foley catheter inserted to drain my bladder and I was gobsmacked to see nearly 2ltr of urine empty into the bag at the side of the bed.
Over the course of my stay on the Neuro ward I was introduced to a flip flow valve, which when inserted into the end of the catheter, have me an element of control over when I emptied my bladder irrespective of whether I had sensation. Most days I would go through something known as Bypassing, where the bladder empties from around the catheter and caused me a huge amount of embarrassment and loss of dignity. Here I was, a grown woman, wetting myself left right and centre. I just had no idea when my bladder was full and would end up having these incidents time and again.
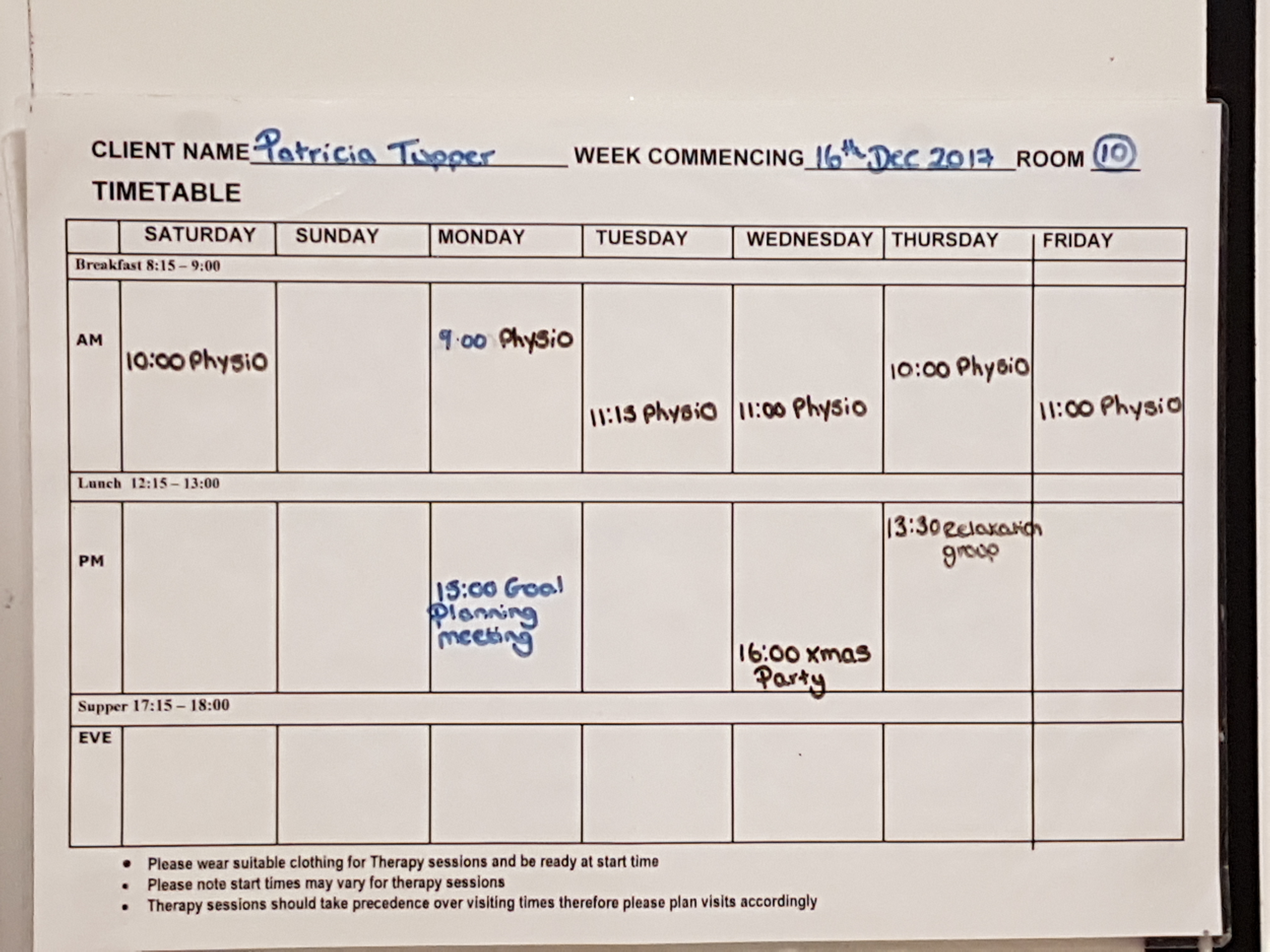
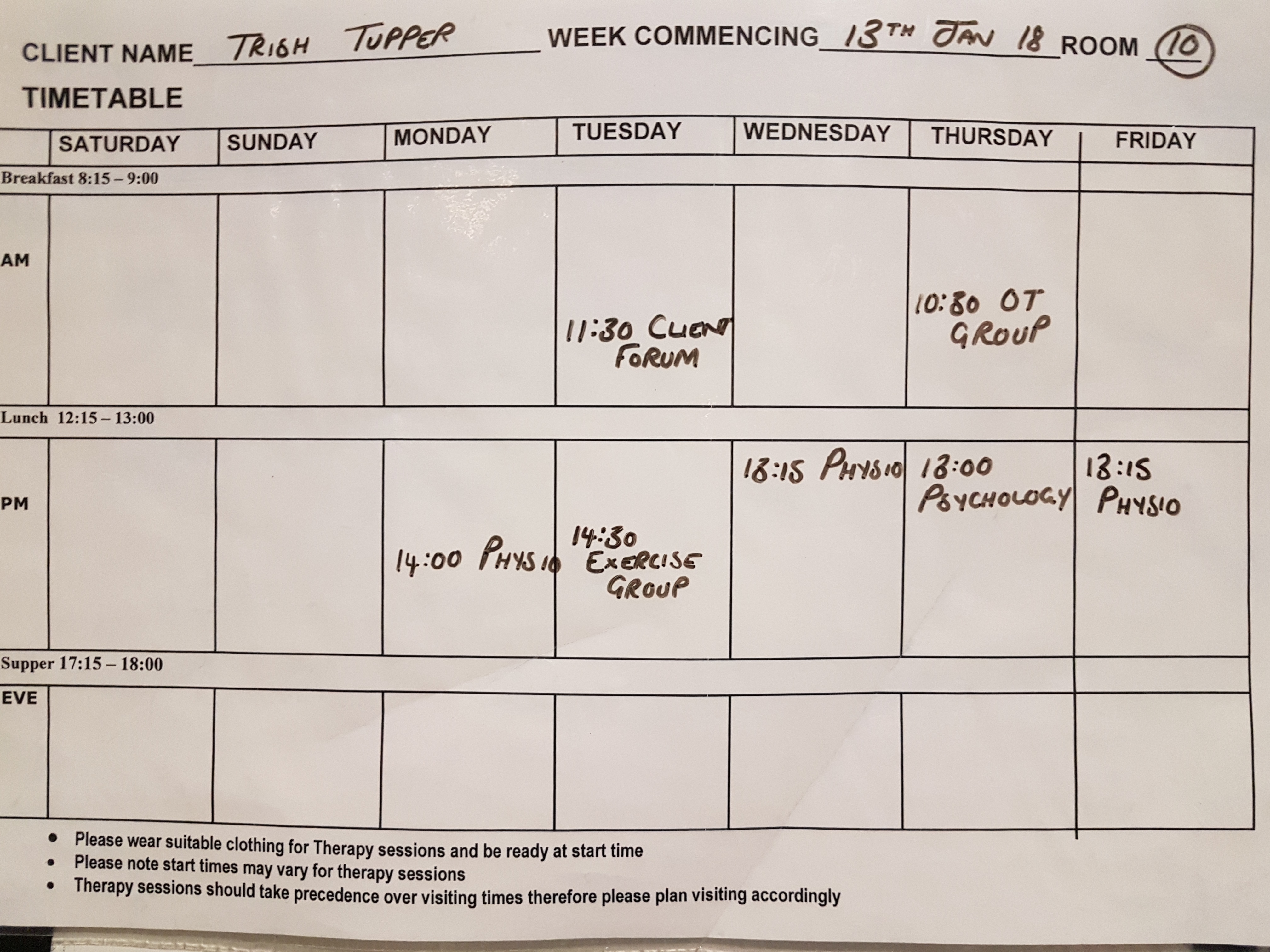
Once I was transferred to the Neuro Rehab Unit I was encouraged to slowly lengthen the amount of time that my flip flow valve was left closed but no matter what I did I just kept bypassing. At one point the doctors wanted to remove my catheter and have a 2 day trial without it (known as TWOC- Trial Without Catheter). I clearly had a lot of anxieties about knowingly wetting myself and having to try and carry on with therapy and social meal times during the trial. I ended up in an hysterical mess which in itself caused more bladder spasms and more frequent periods of bypassing.
I went from wearing normal feminine underwear to big granny pants with discreet pads to then wearing large Tena (other brands available!) high absorbancy pads in a short space of time and began really hating how my body was treating me and why couldn’t I just go for a wee like everyone else.
To add to the humiliation I became doubly incontinent and started having accidents with my bowels. Again due to having no sensation or feeling I would either become constipated, causing palpitations/reflux/nausea, or I would go the other way and pass stools unknowingly and have to face being cleaned up and changed by members of staff. With a lot of time spent sitting on the loo O did manage to get some kind of routine going but it was 50/50 as to whether I would be successful in opening my bowels when I tried.
I can tell you now that 2 years on I still feel utterly humiliated every time I wet myself or have accidental bowel movements, more so embarrassed when I have to ask my husband, or someone else (even my sister in law has helped) to help clean me up.
Just under a year after having my foley Indwelling Catheter (IDC) inserted I was referred to the urology team at University Hospital Southampton Foundation Trust (UHSFT) to discuss what had happened, been going on and where we went next with managing my bladder issues.
The consultant was absolutely brilliant. He listened to what had happened from my perspective, discussed the causes -TM & MS and how the lack of signals through my spinal cord had caused my body to no longer recognise that my bladder is there, and then moved on to what would be the next step.
To say I was shocked by his recommendation would be an understatement. 1st be offered to insert a Suprapubic Catheter. Tbis is where a surgeon creates a hold through your abdomen (normally around your pubic bone) and pass a foley catheter straight through to your bladder. Tbis would mean no more tube hanging down my leg, no more lack of dignity in changing it and a much better option as I am a full time wheelchair user and would save getting caught in my wheels. This suggestion alone had me smiling inside. I hated my IDC with a passion but it was a means to an end.
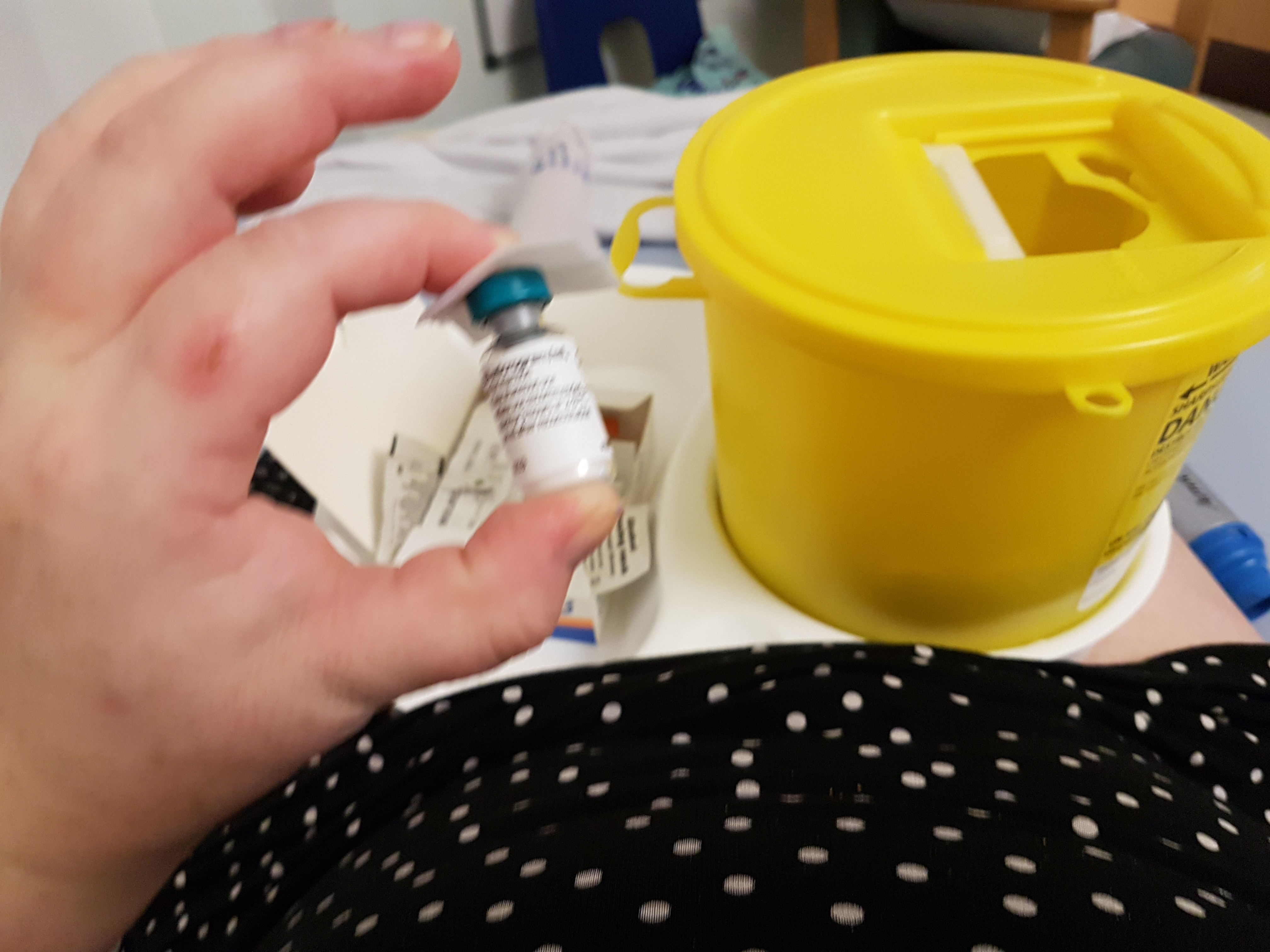
His next suggestion completely threw me out as it wasn’t something I’d ever heard of in this use. He suggested that I was a suitable patient to receive botox into my bladder to try and stop the spasms and reduce my chances of bypassing urine through the usual route. BOTOX!!?? I only ever assumed it was used for cosmetic reasons and was very costly yet here was a kind urologist offering to use this expensive medication to help me in a way i didn’t think possible.
I jumped at the chance to have both procedures done and was put on the waiting list for one of the clinics. We decided there and then that I would have the whole lot done under local anaesthetic due to my lack of sensation and it would mean I’d be home within hours.
It was 8 months before my appointment came around and in that period of time between the decision and appointment I had my IDC fall out 5 x in 8 weeks with the balloon fully inflated. I can assure you it was a pretty scary sight seeing a whole catheter fall out followed by a flood of urine that never seemed to stop! God only knows how many times I called out my District Nurses to come and reinsert a New catheter at varying times of dy and night,or for them to come and give me a bladder wash out because my cathermter wouldn’t drain properly. I gave up feeling embarrassed as it happened all too often.
The day I had my procedure done couldnt come soon enough and desire the fears of being awake I was feeling positive about how my quality of life was about to change.
I watched on in amazement as the surgeon injected the site of the new catheter and my bladder with local anaesthetic and both hubby and I spent the whole procedure laughing with the HCAs whilst they delicately injected my bladder 17 x with botox. It was fascinating watching this needle delicately inject me through a scope with such precision and delicacy
The next part I couldn’t watch. The part where the surgeon pushed an enormous needle through my abdomin into my bladder follows by inserting the foley catheter. Admittedly they couldn’t get it in exactly the right place due to my 2 previous caesarian sections so he had to put it in the fold of my rather expansive belly. Not ideal as its a moist area but it was in and draining like a dream.
I haven’t regretted that decision once and am waiting for my next botox session as my bladder has started fighting against me and I’m having small bypasses regularly throughout the day. I feel like I have my dignity back with regards to my bladder situation.
Now my bowels! They really are causing me a lot mental anxieties.
Due to being on a lot of medication, most of the professionals involved in my ongoing care, at one time or another, have introduced some sort of laxative to try and regulate my bowel movements. Despite trying to self regulate and spending 3+ months on iron supplements, I have found it increasingly difficult to prevent constipation and I’ve ended up really bloated (looking like I’m 9m pregnant- and yes people have asked me when I’m due!!)
This is embarrassing enough without then adding in the humiliation of pooing myself with no knowledge of it and having to rely on people to have to clean it up. I think I’d rather have the constipation over the accidents and it’s something ive never really come to terms with. This admission has helped with trying to find a suitable toileting pattern and a discussion with my consultant lead to me having all laxatives removed and told they’d let me go max 3 days without a bowel movement and then I’d be given something gentle and subtle to encourage a motion.
So far no accidents and a BM a day/every 2nd day. I’m happy with that and just pray that when I go home this pattern continues and I don’t have to go through the humiliation of asking my husband to clean me up.
It intrigues me how differently all these professionals approach both subjects and I know I am just one in thousands who go through this but I’m glad i have the trust in my consultant to do whats best for me and not the text book approach
Enough potty talk now
TTFN











You must be logged in to post a comment.